One week ago, my mom received a phone call that would upend our lives.
“You have a very serious bacterial infection in your lungs,” her pulmonologist said, “but it can be treated.” He explained that it’s Pseudomonas and said he would prescribe an antibiotic for her. “It’s important to treat it before it becomes more serious.”
He was going to give her levofloxacin but noticed the records said she’d had a bad reaction to it.
“It was hard to describe the feeling it gave me,” my mom later told me, “but it scared me, and I was afraid to take any more.”
Her pulmonologist said they could try ciprofloxacin (cipro). If her body doesn’t tolerate that, she would have to go into the hospital, where they would administer an antibiotic intravenously for seven days.
After my mom called me, I rushed to research alternatives to cipro because I was already aware of its potentially lethal and debilitating adverse effects.
I called to speak to her pulmonologist. His medical assistant served as a go-between while I asked about alternatives and played through various scenarios so I would be prepared for each possibility. When I asked what they might prescribe at the hospital, they couldn’t tell me because that would be determined by the admitting hospitalist.
Given the premise that this was a life-threatening infection that needed to be addressed quickly, it seemed the only option was to brace for a ten-day course of cipro while my mom stayed with me so I could monitor her for reactions.
I begged my mom to wait while we researched alternatives.
“I feel like my back is against the wall, and I have no other choice,” she told me.
After imploring me not to let my mom take cipro, which she is fairly certain killed her friend shortly after his starting it, a dear friend wrote me:
“I detest the urgency that doctors put patients under, when it isn’t always warranted. Yes, it may be a serious condition that you have just discovered, and the Drs can tell you many scary stories, but that doesn’t mean this is what your mom will experience. If she has been maintaining for many months, and it has not gotten substantially worse, then I would take a deep breath and consider whether you can both take a few days to do as much research as you can, talk to Mike, get your mom settled and comfortable in your home, etc. Try the nebulizer.
“I also know that it’s not just you making decisions, that your mom has some say. But then it can be difficult if she might not want to read the side effects, and she might not understand how dangerous medical care is these days, etc.
“Just know that most likely you can take a deep breath, pause, think, ask more questions, consult others, get a second opinion.”
And that’s exactly what I did.
Even though my mom needed the peace of mind of a settled decision (the plan to take cipro while staying with me), I wasn’t going to give up. My gut told me to do whatever I could within my power to save her from cipro, even as I tried to counterbalance the terrifying experiences relayed to me by friends with those of others informing me they had taken cipro without major side effects.
Thanks to what I now believe is the divinely orchestrated incompetence1 of Walgreens, my mom’s prescription for cipro wasn’t filled until the Monday after her diagnosis.
That gave me five days to research and confer with trusted doctor and scientist friends around the world.
One of those was Dr. Mike Yeadon, whom I love like a father, brother, friend, mentor, and colleague all wrapped into one. After a riveting hour-and-a-half–long conversation2 that soothed my heart and invigorated my mind, we reluctantly bid farewell.
The phone rang a moment later. I’d forgotten I’d temporarily turned off Silence Unknown Callers. I almost pushed the button to send it to voicemail, but then I noticed the New York area code.
“Hello?” I picked up, wondering if it was the person I hoped it was as he had told me the previous day he would call me.
“Hi Margaret,” Dr. Pierre Kory said. I felt a wave of relief wash over me.
Early Saturday morning, I had shared my Substack Note about my mom’s original diagnosis and emailed Pierre this message:
“Pierre, I would be grateful to speak/text/email with you if you can offer any insights on my mom’s treatment for pseudomonas aeruginosa (with the additional complication that she has lupus) and perhaps offer reassurance that we made the right decision by going with Cipro (despite its horrendous safety profile) while having her stay with me during treatment so I can monitor for potential adverse effects. Backup plan is the hospital w/ IV antibiotics if she does have a bad reaction, but that’s a last resort as hospitals are murder centers and also notorious breeding grounds for pseudomonas!”
He asked for my cell and said he would call me when he was free.
That night I followed up with some additional findings from my research that day:
As I mentioned in my previous email, I am listening to The War on Ivermectin, and your mentioning of intravenous vitamin C got me wondering if it would be useful for treating Pseudomonas aeruginosa—and voìla! I found a promising study right off the bat:
Assessment of Antibacterial and Anti-biofilm Effects of Vitamin C Against Pseudomonas aeruginosa Clinical Isolates (published in Frontiers on Microbiology)
This part caught my eye:
“The antimicrobial effect of vitamin C exists against the all the P. aeruginosa clinical isolates tested. To our surprise, vitamin C inhibited the growth of P. aeruginosa clinical isolates at lower concentration ranges of 156.2–1,250 μg/ml, while MIC50 and MIC90 were 312.5 and 625 μg/ml, respectively.”
I am very curious to get your thoughts on using intravenous vitamin C in conjunction with cipro and perhaps other treatments. Also wondering what you think about H₂O₂ nebulization for this purpose.
I found this presentation very informative and am wondering if inhaled antibiotics (tobramycin, aztreonam, gentamicin, or colistin) are now approved for usage and if they would be a viable alternative to oral cipro or if they should be reserved for long-term cases (>3 years) as indicated in the presentation.
For oral cipro, the presenter says the European Respiratory Society determined the optimal duration is a minimum of 14 days, but my mom’s pulmonologist only prescribed 10 days. This could be because the presenter is focusing on this in the context of patients with bronchiectasis, though, so perhaps 10 days is appropriate for my mom since she doesn’t have that.
And what about nebulized colloidal silver? I know Dr. Jackie Stone (RIP 😭) had great success with incorporating nanosilver into her protocol.
Curious about your thoughts on ozone therapy, too. And molecular hydrogen (sorry if I’m overwhelming you 😁).
I have been corresponding with Dr. Ross Pelton, The Natural Pharmacist and the husband of a longtime client/friend I just happened to meet in person recently and who has generously provided guidance—including sending a bottle of what he considers the world’s best probiotic, Dr. Ohhira’s Probiotics, for my mom to take two hours after each antibiotic dosage and then to continue after she completes her course of cipro.
Here are Ross’s thoughts on H₂O₂ nebulization and molecular hydrogen:
“Hydrogen peroxide inactivates microorganisms (bacteria, yeasts, fungi, viruses, and spores) through oxidization. However, it must be used wisely. Too much (or too strong a concentration) can be harmful.
“Actually….molecular hydrogen has more health benefits than taking hydrogen peroxide. My good friend Bob Settineri wrote the book on molecular hydrogen.”
This is the book he referenced. Unfortunately, it’s only available directly from his website, so I haven’t gotten it yet.
Also just came across this article re: niclosamide while researching to see if ivermectin might be useful for this:
“In Gram-negative bacteria, only niclosamide exhibited antibacterial activity. This drug showed an anti-virulent effect against Pseudomonas aeruginosa via the inhibition of quorum sensing and virulence genes, reducing elastase and pyocyanin levels.”
Other drugs that have shown promise include albendazole (AbZ), citral + triclosan, and metformin as well as bioactive phytochemicals and the antioxidant lignans sesamin and sesamolin (found in sesame).
Now I probably am overwhelming you, so I’ll stop there :-)
I guess what I’d like to know is if this were your mom, what protocol would you assemble for treating her to maximize the chances of successful eradication of Pseudomonas while minimizing potential toxicity from antibiotics such as cipro?
If you haven’t read my Substack Note with more details about my mom’s case, I wanted to make sure you are aware she also has lupus, Sjogren’s [syndrome], and Hashimoto’s, further increasing her vulnerability.
What’s funny is those questions turned out to be moot because the premise that Pseudomonas was causing her chronic cough was faulty.
During our forty-five–minute phone call, Pierre wielded questions like a samurai swordsman, deftly cutting to key details for further elucidation until he had a clear picture of my mom’s symptoms, diagnosis, history, and other conditions.
“The pieces aren’t adding up,” he repeated several times.
“As someone who’s an expert in chronic cough, I have never come across a case of Pseudomonas that caused a chronic cough,” he said. “This would be the first case I’ve seen in twenty years of practicing.”
He explained that yes, the respiratory culture shows it is present, but that’s not what’s causing her chronic cough. In the rare cases where Pseudomonas is a threat, it manifests as an acute illness, not a chronic one. In other words, the symptoms would be so severe, my mom would be in the hospital fighting for her life.
So we started digging down to uncover the underlying condition responsible for her chronic cough.
I didn’t know this at the time, but Pierre had already formed an opinion. He didn’t want to say it aloud until he saw her imaging results to confirm his hypothesis, though.
“Infections are typically unilateral or asymmetric,” Pierre explained during a follow-up exchange. “Autoimmune and/or inflammatory conditions are generally symmetric. Obviously, there are exceptions to both, but the above patterns are the most common. And that is why I was so interested in seeing her CAT scans. I was particularly interested in the pattern of distribution and involvement.”
“I was considering that this could be a complication of or direct result of a lupus flare,” he texted later. “That is why I wanted to see if there was symmetry involved.”
After we got off the phone, I texted him, and the following mind-blowing exchange ensued:
MAA:
Thank you for your phenomenally insightful and generous call this morning, Pierre. You are a rockstar 😎 It was such a delight to finally speak with you in person! For the scans, you need to see the actual imaging, right? I have been scouring MyChart but have only found reports with descriptions so far. I started going back through her summer 2018 records from when she was hospitalized for pneumonia and system[ic] inflammatory response syndrome (SIRS), and I discovered they found mycobacteria: M. abscessus subsp. massiliense. Now I’m starting to wonder/worry if it is MAI 😬
PK:
that is exactly what I was saying. And although I would love to see the imaging, I will take an imaging report for sure I can work with that.
MAA:
Let me try to track those down and transcribe the findings. I downloaded so many files, now I have to find them again 😆
PK:
sounds good
MAA:
This is going to sound really weird, but is there some sort of lung disease with “Lady” in the name, like a Victorian-sounding name? I remember when my mom got her CT scan results that summer, there was a report in there that made me so worried, I brought it to my pulmonologist, and he was concerned, too. I kept telling my mom she needed to follow up on it, but her doctors never did anything further related to it. I think there may have been a fungal infection. I remember doing research and coming across the name of a condition that appeared to match, but I have been racking my brain trying to remember it, and all I can think of is “Lady” some name is in it.
Two minutes later, I wrote:
OMFG. I just searched my bookmarks and found Lady Windermere Syndrome!! That is it!
I bookmarked this article.
PK:
The entire time I was talking to you, I was thinking that this was most likely Lady Windermere Syndrome
MAA:
I’m getting chills.
Whoa, I’m reading that article, and this is my mom exactly: “No one has figured out why thin elderly women seem to be at greatest risk for infection from this normally pretty feeble bacterium.”
PK:
yup.
A few beats later, I told him, “I love unraveling medical mysteries like this—if only it weren’t my mom.”
Now that I had the date of the 2018 CT scan report, I decided to hunt through my Sent emails and found a note I emailed my mom on October 22, 2018, at 7:28 pm:
“It’s a little worrisome, but I did find that the tree-in-bud pattern can be associated with Sjogren’s. It may also be related to the lupus. Or the mycobacterium or aspergillus. You’re such a mystery!”
This was followed by a report of my findings the following evening at 10:16 pm:
“While I was [at my pulmonologist’s office], I asked if he would be willing to look at your CT scan. He very generously spent several minutes reviewing it and said you definitely need to see a pulmonologist about the MAI (Mycobacterium avium-intracellulare infection). He said it is unlikely to go away on its own and that you may need to be on three different antibiotics for a couple of years :-( It progresses slowly, but you don’t want it to get to the point where it compromises your lungs. When I mentioned they originally thought it was TB, he said it is actually atypical TB (non-contagious, fortunately), but I got the sense that it’s less threatening, thankfully. He also wasn’t concerned about the aspergillum.
“He said there’s a pulmonologist up at OHSU experimenting with a treatment for MAI that isn’t as drastic as the long-term multi-antibiotics treatment. I could try to find out the contact info if you’re interested in that, but it would probably involve travel to Portland and multiple visits, so I’m not sure if you’re up to that. Then again, a few short plane trips would be worth it if it saved you a couple years on antibiotics!
“Most people have mycobacterium in their bodies, but only people with compromised immune systems are susceptible. Your lupus flareup probably made you vulnerable to it, and it was able to start growing, and the mycobacterium is probably what caused the pneumonia (that is one of its potential side effects). It’s possible the steroids enabled it to grow more in the meantime since they suppress your immune system (this is my guess based on what I’ve read about mold).
Dr. F— didn’t mention this, but after doing research, I think it may be Lady Windermere syndrome. It tends to strike thin, frail, older women (never-smokers), often with scoliosis. I think you should mention this syndrome to Dr. G—, M—, and the infectious disease doctor (sorry, I can’t remember her name!).
Dr. F— agreed your primary care doctor should be an internist or someone with enough expertise to address your range of symptoms. Have you followed up with M— about that referral yet?
When are your next appointments with Dr. G— and M—? And have you heard anything from the infectious disease doctor? I think you need to call all of them (let me know if you need me to help) and tell them about Dr. F—’s concerns and the possibility that this is Lady Windermere syndrome. You need to get a referral to a pulmonologist ASAP because it can take months to get in (Dr. F— said the wait isn’t quite so long now as they have a couple additional pulmonologists on staff now, thankfully). And you should see the infectious disease doctor ASAP, too, as she may feel it’s time to start you on treatment to halt the MAI’s progression.
The first and most immediate thing you can do, though, is consume lots of apple cider vinegar! I came across this article about ACV killing mycobacteria (including TB!). It also helps regulate blood sugar levels. Here are some articles on its uses and benefits:
https://www.thehealthsite.com/news/vinegar-a-natural-remedy-for-treating-tuberculosis/
https://www.livestrong.com/article/535407-will-apple-cider-vinegar-cure-a-bacterial-infection/
Ideally, you would be able to treat the MAI naturally with ACV and perhaps other remedies. Coconut oil is antimicrobial and antifungal as well. You could at least start consuming them so you’re taking action immediately while waiting for doctors’ appointments and more details on treatment.
I initially lamented that my mom’s doctors had failed to properly monitor her lungs and follow up on the presence of mycobacterium and the tree-in-bud pattern in her CT scans, but I realized in retrospect this spared her from the traditional treatment of two years on three aggressive antibiotics, which would have decimated her gut health and consequently her already-malfunctioning immune system.
While researching alternative treatments for lung infections, I found one that kept coming to the surface—chlorine dioxide (see also MMS).
I had never heard of it until a friend mentioned it to me a few weeks ago. Then, the morning I talked to Pierre, he and two other people informed me about its clinically impressive outcomes. I have yet to research it myself, but what I’d heard about its apparent safety and amazing efficacy for a broad range of conditions intrigued me.
Indeed, Pierre just launched a new series on chlorine dioxide, so I encourage you to read this and subscribe to his Substack for future entries.
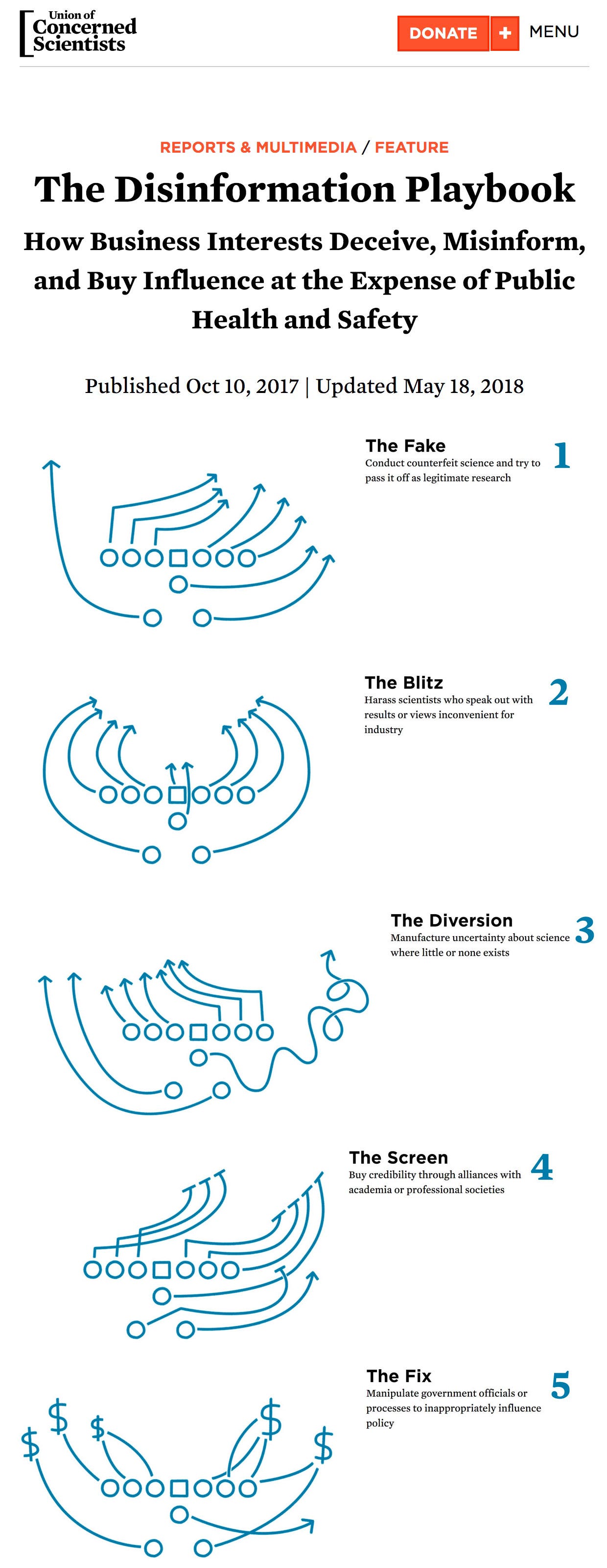
Since there is no greater threat to Big Pharma than a cheap, readily available substance that is highly effective for a wide range of conditions and has minimal to no side effects, the propaganda and censorship machine has already locked its sights on chlorine dioxide, deploying the standard Disinformation Playbook. Only this time, Pierre told me, they’re going even further—instead of just discrediting and burying studies, agencies are actually preventing them from being conducted in the first place. Fortunately, there are some countries where scientific freedom still exists, mostly in South America, it seems.
I emailed myself a note that night to ask Pierre if it might be appropriate to use chlorine dioxide for treating my mom’s conditions.
Once again, we were thinking in parallel because I received this text from him before I got a chance to ask him:
“yes, it would appear3 that your mom has some sort of non-tuberculous microbacteria [mycobacterium], it could be MAI or it could be a cousin of MAI, but either way now that she is persistently symptomatic it merits treatment. The problem is that there is an old adage about MAI: ‘it becomes a disease of medicines’ because they are poorly tolerated. I personally would pursue a chlorine dioxide protocol, likely via nebulizer with or without oral administration as well. there is a trial going on in Ecuador for drug resistant TB using chlorine dioxide, I will try to find their protocol if you guys are interested.”
I replied:
“Thank you, Pierre!! You read my mind as that is what I was going to ask you about! I would be grateful for the protocol 🙏🙏🙏”
“Since it isn’t life-threatening immediately, I was going to recommend to my mom that we pursue alternative protocols first. I think she would be very grateful to avoid years of antibiotics!”
“That should take care of the pseudomonas, too, right? Not that it’s causing her issues but would be nice to do in one fell swoop.”
He confirmed it would take care of both.
I told Pierre:
“You may have saved my mom’s life or at least her health from the ravages of two years on three antibiotics! I will be forever grateful to you, Pierre 🙏”
After getting some much-needed sleep (having stayed up for twenty-nine hours the day we got the Pseudomonas diagnosis and then another twenty-eight hours after mind-melding with Pierre and embarking on another monomaniacal research quest), I forwarded Pierre’s text to my mom at 12:20 pm on Monday.
My phone rang a few moments later.
“I was just about to walk out the door and pick up my cipro prescription!” my mom said.
We then spent the next twenty-two minutes basking in what felt like a series of miraculously synchronized events engineered to save my mom from cipro and point us toward chlorine dioxide as a healing solution.
If Walgreens hadn’t taken five days to fill the prescription … if I hadn’t connected with Pierre to get a second opinion … if multiple people hadn’t started telling me about chlorine dioxide all at the same time … if the Ecuadorian clinical trial with a near-match for her condition wasn’t underway … if her doctors had given her the traditional treatment six years ago when I first identified Lady Windermere syndrome … if … if … if …
So many different ifs could have led to a fatal or crippling outcome, with my mom potentially suffering lifelong health consequences from cipro or, worse, a two-year course of triple antibiotics.
When I updated her about what was happening with my mom, one of my oldest, dearest real-life friends, Tracy, wrote:
“Don’t let her have Cipro. It incapacitated me for 2 months. Joint swelling and I could barely walk and had 22 cc of fluid taken off one knee. It’s horrendous and robs your body of magnesium absorption for years after!”
One of my readers, Xingyi, also shared his brutal experience with cipro:
“I have started telling all doctors that I’m allergic to all fluoroquinolones — of which levo and cipro are common examples. I have been injured by both BTW. I’d say fairly seriously.
“The levofloxacin injury included damage to the tendons in my left foot amongst other issues as well. But that one is relatively permanent. The bone doctor informed me that I have serious ‘lesions’ on my tendons because of it.
“I have been injured by both oral ciprofloxacin and Ciprodex ear drops. The former sent me to the hospital in anaphylaxis. The latter, in order to treat ear infections, has (come to find out) drastically damaged and reduced my hearing.”
Now, instead of feeling like I’m stuck in a bad dream watching an oncoming train hurtle toward my mom while she’s tied to the tracks and I am fumbling to untie the knots, I feel grateful, excited even. As I texted Pierre:
“I’m actually really excited about embarking on an alternative therapy protocol as it could help many others if this works for her and I share the journey.”
This truly felt like a Christmas miracle, and perhaps it was, thanks in part to hundreds if not thousands of people around the world having joined in prayer to support my mom, with special gratitude to TriTorch for the following poignant prayer request at the Coffee & COVID (C&C) community:
“I had the luxury of speaking with the great Margaret Anna Alice yesterday evening. After being awake for over 24 hours she had just learned that her mom is quite ill. They have some difficult and dangerous choices to make. She is devastated. Hat in hand, I ask for yet another prayer: please pray for them both.
“All of this sadness that surrounds us in this dwindling age got me thinking about love and death and life. Here is an arrangement of quotes as a thank you for your blessings and grace … [truncated due to space, but I do encourage you to read the original comment in full as it is beautiful]
“Yesterday, after only few brief paragraphs of explanation of what she just found out her mother was facing, an exhausted and grief-stricken Ms. Alice then apologized for ‘unloading her problems on me’. Can you imagine? Please pray for Ms. Alice. She fights for us, let us fight for her.”
Thank you, brave readers, for fighting for me—and especially for my mom, whom I could not bear to lose under any circumstances but especially after losing Michael.
Please spend this Christmas—and every day thereafter—cherishing with all your fully present being everyone you hold dearest in your life.
I know I will—and that includes each one of you blessed souls who cares enough to read my words and use them in our shared mission to radiate truth, light, and love across this bedraggled globe.
© Margaret Anna Alice, LLC
🙏 Thank You for Lifting Me Up
I want to thank the 1.56 percent of you who pay for a subscription 🙏 To the remaining 98.44 percent, please consider subscribing. Substack is how I survive.
Will you help me by subscribing or making a one-time donation?
You may not think your few dollars a month makes much of a difference, but every dollar absolutely helps—not only financially but also emotionally as it shows you feel my content is worth supporting.
When you subscribe, you gain access to premium content like Memes by Themes, podcasts, Consequential Quotes, Case in Point, Behind the Scenes, Dissident Dialogues in progress (“rolling”), personal writings, and bonus articles.
😇 Become a Founding Member
If you take the extraordinary step of becoming a Founding Member, you will enjoy benefits such as:
signed & personalized copy of Canary in a Covid World
special gifts
select typeset PDFs
Zoom call
I especially want to thank those of you who have taken the time to write a private message to me when you subscribe. I read and cherish each note.
Thank you for being part of our karass of brave, brilliant, kind, and witty thinkers.
🤲 One-Time Support
🙏 Shoutouts Gratitude
🛒 Spread the Words
If you would like to help propagate the message that Mistakes Were NOT Made, you will find a wide selection of products in this collection.
📖 Get Signed Copies of My Book
The holidays will be here in a flash, so now is the time to stock up on signed, personalized copies of my fairy tale for your loved ones. It makes for a thought-provoking, accessible gift whether they are awake or asleep, adults or children.
📚 Anthologies
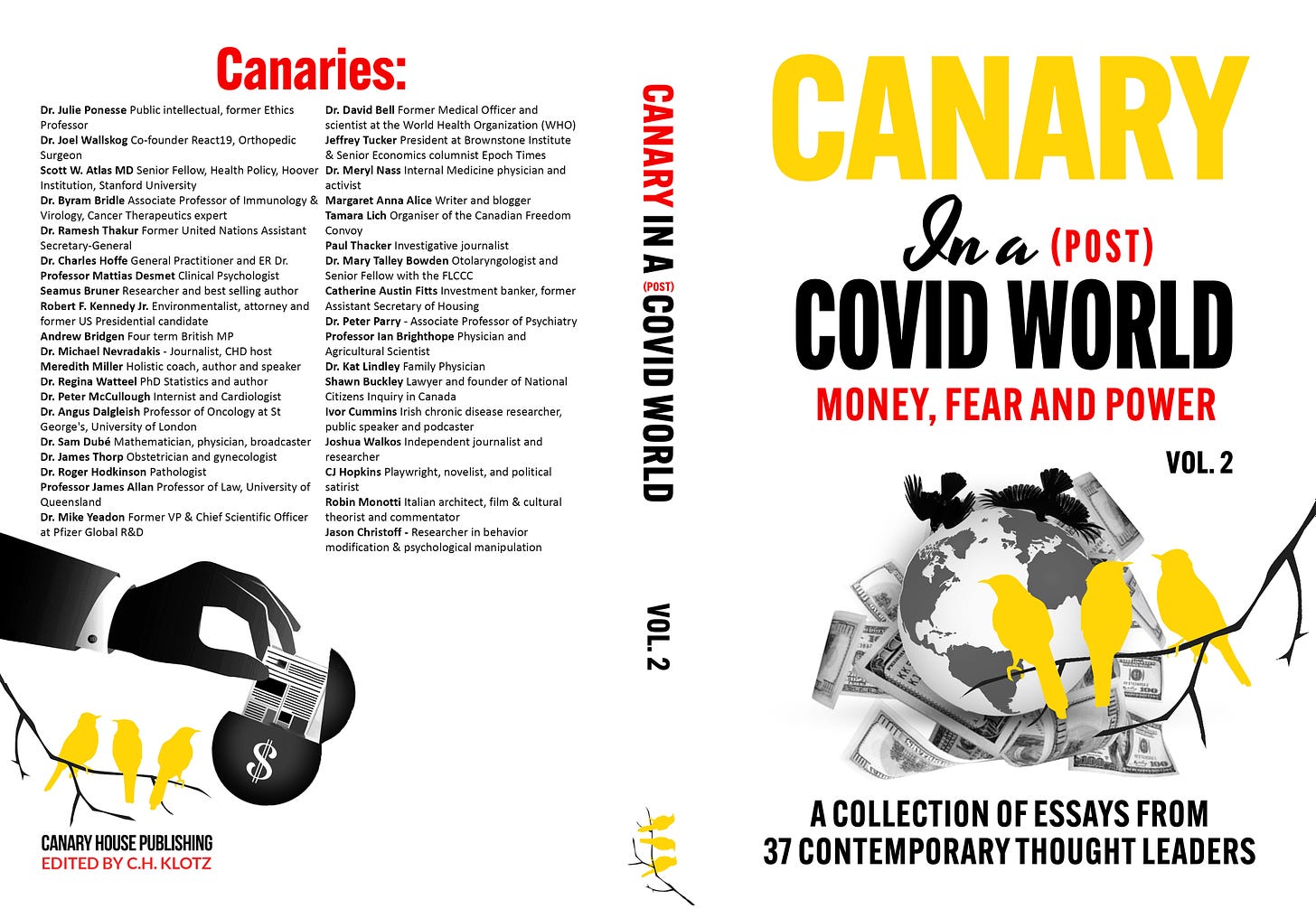
Canary in a (Post) COVID World: Money, Fear, & Power (Hardback, Paperback, Kindle)
The second volume in the Canary series just dropped, and I am grateful to be a contributing author once again.
Canary in a Covid World: How Propaganda & Censorship Changed Our (My) World (Paperback, Kindle, Audiobook)
Yankee Doodle Soup for the Fringy, Tin Foil Hat–Wearing Conspiracy Theorist’s Soul
Edited by Jenna McCarthy, this hilarious anthology includes Letter to a Mainstream Straddler and Letter to Klaus Schwab. The paperback is only available for purchase at her website. If you enter the code ALICE at checkout, Jenna will give me a royalty 🙏
A Doctor’s Despair (Paperback, Kindle)
🐇 Follow Me on Social Media
⏰ Wake-up Toolkit
My Wake-up Toolkit is a great way to get acquainted with my content. I’ve organized my articles by topic for easy reference and use in your red-pilling efforts as needed. Note that I have not been able to update this since June 2024 due to a technical issue, so check my archive for more recent additions.
🌟 WARM GRATITUDE FOR THE RECS!
The single-most important driver for new readers joining my mailing list is Substack Recommendations. I want to thank every one of you who feels enthusiastic enough about my Substack to recommend it, and I especially appreciate those of you who go the extra mile to write a blurb!
Remember, a subscription to Margaret Anna Alice Through the Looking Glass makes for an intellectually adventurous gift down the rabbit-hole!
Note: Purchasing any items using Amazon affiliate links included in my content will further support my efforts to unmask tyranny.
While reviewing this draft, my mom noted, “Walgreens wasn’t exactly incompetent, but they were out of ciprofloxacin, therefore the delay.” Okay, so it was a divinely orchestrated inventory shortage, but that’s not as pithy as “incompetence” ;-)
Prior to calling, Mike had provided the following thoughtful analysis in response to my questions about my mom’s condition and proposed treatment, having first clarified, “I’m not a medical doctor. Your mom’s health is not for making uneducated guesses about. I’d recommend a trusted, ‘awake’ doctor, but I know so few that I’d truly trust”:
Glancing at the respiratory culture result, presumably on sputum (coughed up material) I noticed polymorphonuclear leukocytes. PMNL are also known as neutrophils. They’re bacteria killers, defensive cells that arrive in numbers of bacteria get out of hand.
They are THE cause of pus in wounds in skin for example & in lungs, they are wholly responsible for the disgustingly coloured mucus a person can cough up.
Paradoxically, this is a positive sign. It shows your defence system is doing its job.
Usually, if the defences are strong enough, supportive care and good nutrition permits them to clear the inappropriate overgrowth of bugs.
So whatever you’d normally do to support a healthy immune system, I’d continue to do that.
If there are chances to sit somewhere in sunshine, perhaps in a glasshouse if it’s cold, I think that’s better for recovery than being confined to bed, which is really not ideal. Bed rest can sometimes be unavoidable but I’ve long believed it to be really quite dangerous. Our bodies, if not required to support us moving around gently (or vigorously) “de-trains” at an alarming speed. This makes recovery harder because in addition to healing whatever’s caused their immobility, their body has to regain its lost strength due to bed rest.
I’ve asked the one doctor I know who is also a scientist. The poor man is being legally tortured by a corrupt legal system and judiciary. They intend to destroy him financially and he’s even seen messages between coconspirators that they won’t rest until he kills himself. All because he told the truth about deliberately dangerous medical practices and injurious injections.
So he may not be able to get back to me.
Personally I’ve taken cipro several times for various diagnoses infections. Perhaps chest, gum and jaw & also urinary bladder. It’s always given me abdominal discomfort and badly affected bowel habit, but nothing worse. I do recognize that some people do have poor reactions to it but I don’t know if there’s any way to evaluate whether a patient is at risk or not. Probably not.
The big question is “Why has she become colonised by pseudomonas?” It doesn’t just happen by chance & then it’s this that causes symptoms.
I think that there must be something underlying which has allowed this strain to overgrow. She may have had symptoms from whatever is the underlying condition, before the fulminant overgrowth.
While it still seems logical to want to help the body clear the overgrowth, it wouldn’t be unreasonable to expect a recurrence unless something else is changed.
I agree with you that being admitted these days is a higher risk thing than it used to be. There are surprisingly few options in antibiotics. Some aren’t available as oral forms & instead are administered intravenously. An indwelling intravenous line is not generally placed outside of a hospital context, hence the description of “If not cipro, then admission for IV agents is the alternative”.
I recall that ciprofloxacin and it’s analogies have anti inflammatory properties as well as antibacterial properties. So even those favouring “terrain” theory shouldn’t reject these agents out of hand. I’ve long thought it possible that part of their therapeutic value (when observed) could come in part from their anti inflammatory effects. Nobody really knows. You can appreciate that drug companies don’t want to know about this, because they currently have a very good business having huge numbers of prescriptions written for antibiotics. They don’t want anyone suggesting that it might be for a different reason that they work.
If your mom is otherwise in reasonably good health for her age, I feel that prognosis is good.
Consider that she’s had symptoms for weeks to months, which means it’s not an out of the blue medical emergency. You’re giving her all your care and attention & this alone is probably an important part of healing her.
Severe adverse effects that I recall are more likely to the subacute to chronic use situation.
Cipro can be so effective at killing off your needed commensal bacteria in your lower bowel that sometimes there’s an overgrowth with a life threatening bacterial strain. I don’t think that’s at all likely with a single, short course, especially if diet is chosen to be particularly supportive.
There may be other risks but I’m not familiar with their frequency. Being watchful for anything changing is of course very important.
When doctors were incompetently managing my persistent bladder infections in 2016, which arose because of long term urinary retention (which was due to anatomical problems) I think I had six or more full courses almost in a row. I honestly thought it possible to likely that I’d perish because I felt increasingly unwell as well as in pain and nobody seemed to understand what was happening or what to do about it.
In the end, I demanded my last microbiology report. The doctor didn’t to let me have it, but I insisted. Before I’d even reached my car, I saw the problem. The antibiotics I’d been on for two solid months had no spectrum of activity against the organism last cultured from urine. I was furious. The doctors assistant told me a new prescription was immediately available at the nearby pharmacist and two weeks later, I was well again.
Most doctors I’ve had the misfortune to encounter even before 2020 seemed inattentive or even careless. That is my experience anyway.
…
On all the other options, this is distinctly in the field of exploratory medical care.
I simply do not have the knowledge base to comment.
The one thing I’m pretty sure is salutary for our respiratory system is ozone. At the seaside, sunshine and salt water generates a noticeable amount of ozone, which is that seaside smell that is sometimes very distinctive.
There’s a decent old literature that being by the sea is helpful in recovery from respiratory ailments.
After I told Mike about Pierre’s assessment, Mike responded:
OMG! I too wasn’t convinced by the diagnosis but had no alternatives beyond potentially a chronic fungal infestation. I didn’t mention it because I’m painfully aware that I am scientist and not a physician.
A so-called therapeutic trial was and may yet be worth considering. Fluconazole as a single dose is enough because it is cleared from the body only extraordinarily slowly with a half life of days.
There’s a one capsule product called “Diflucan One”. It clears oral and vaginal thrush and also persistent airway infection.
It’s well tolerated so if you later are casting around for alternatives, it may be worth considering.
Amazing that you & a physician had the same idea!
Go, Margaret Anna’s mom ❤️😎😊xxxx
Mike
I just called Mike to get his permission to include these notes, and he closed our conversation by saying, “You’re one of my heroes.” Hearing that from one of my greatest heroes and the man I crowned the King of Integrity years ago left an indelible mark on my heart 💓😭💕
Because mycobacteria take so long to incubate, it can be up to eight weeks before a report is issued. This means the diagnosis is not 100 percent certain until the results for my mom’s respiratory culture arrive. Pierre also made this clarification during a follow-up exchange:
“MAI [Mycobacterium avium-intracellulare infection] and NTM [nontuberculous mycobacteria] are still at the top of my differential diagnosis after seeing the chronicity and descriptions within her imaging report.”



























Antibiotics all wipe out healthy bacteria and lower future resistance to any kind of 'bug' that comes along. There are natural remedies such as, Golden seal root, which worked wonders for my own daughter, when she was so sick that she could not speak. Within hours, she was able to talk. My friend was ready to put her daughter in the hospital, but I told her to ask her doctor if she could wait until the next morning. He said that it was alright. Well, my friend started giving her the Golden Seal Root every few hours along with warm lemon and honey...and she was better the next morning...no more problem. My aunt had a cough that persisted for years from something she ate daily...grapefruit. She would not give it up...and did not live. My friend was very ill a couple weeks ago and ready to go to the hospital. Many of us prayed for her...and she took some natural remedies and went to sleep. The next morning she was better. All my life I have depended on common sense...which means eating natural food, not processed..and prayer.
I follow the guidance of healthy older people who told me years ago, if you want to live long and be healthy...keep out of doctor's offices. I listened to their advice and I'm healthy at 90..
Cipro and Keflex are horrid nasty things. In my life of 76 yrs, Cillin's are the only antibiotic I can tolerate. From Penicillin to Amoxicillin. NO Mycian's either. You can add steroids to the list.
Glad you did your home work.